Abstract
Background: Cancer patients are considered to be prothrombotic with major disturbances in hemostasis that are associated with an increased risk of venous thromboembolism, especially in patients with advanced cancer. Recently reports show that the high levels of circulating microparticles (MPs) have procoagulant activity (PCA) in oral squamous cell carcinoma (OSCC). However, this study did not address the question of what specific mechanism might underlie the PCA in OSCC. Neutrophil extracellular traps (NETs) are activated neutrophil-derived web-like structures, which have emerged as important mediators in cancer progression, metastasis and cancer-associated thrombosis. Additionally, the cytokines and neutrophils were known to become aggregated in cancers and are usually present in high numbers in OSCC patients and are associated with poor outcomes. The exact molecular mechanisms responsible for modulation of neutrophils procoagulant functions in OSCC are, however, poorly understood. Thus, we hypothesized that cytokines might activate neutrophils to release NETs, thereby predisposing OSCC patients to a hypercoagulative state. Moreover, we evaluated NETs interaction with human umbilical vein endothelial cells (HUVECs) and their association with pathological lesions in this disease.
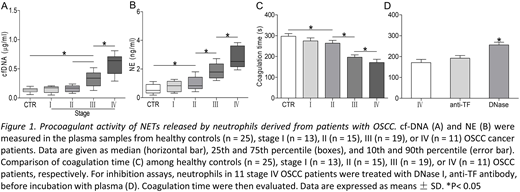
Methods: OSCC patients (n = 58) were divided into four stages according to the 2009 guidelines of the American Joint Committee on Cancer staging classification, and compared to healthy controls (n = 25). Cell-free DNA (cf-DNA) was quantified using the Quant-iT PicoGreen dsDNA Assay Kit. ELISA was used to detect MPO-DNA complexes, TAT (thrombin-antithrombin) complexes, neutrophil elastase, nucleosomes, and cytokines. PCA of NETs was evaluated using coagulation time and purified coagulation complex and fibrin production assays. Phosphatidylserine (PS) exposure, fibrin strands, and FVa/Xa binding on cells were observed using confocal microscopy.
Results:Plasma levels of NET markers in patients with stage III/IV OSCC were significantly higher than those in stage I/II patients or controls (all p<0.05), and positively correlated with thrombin-antithrombin (TAT) complex and fibrinogen levels. Interestingly, neutrophils from OSCC patients with stage III/IV were more prone to release NETs compared to those from stage I/II patients and controls. Additionally, we found that plasma from patients with stage III/IV OSCC was able to prime neutrophils to generate higher amounts of NETs than from stage I/II patients and controls. Depleting IL-8, IL-6 and TNF-a reduced plasma-enhance NETs release. In addition, NETs released by stage III/IV OSCC neutrophils significantly increased the potency of control plasma to generate thrombin and fibrin, greatly shortened the coagulation time (all p<0.05). These effects were attenuated by DNase I. Finally, isolated NETs induced ECs to lose normal morphology and retract from their cell-cell junctions, converting them to a pro-coagulant phenotype. DNase I attenuated this cytotoxicity.
Conclusions:These results suggest that OSCC creates a systemic inflammation environment that primes neutrophils to release procoagulant NETs in patients with stage III/IV OSCC. The NETs formation correlated positively with the parameters of disease severity. The information that results from these investigations may serve as a rational basis for the design of future drug intervention trials that target coagulation reactions, mechanisms and/or interactions relevant to OSCC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal